The examination itself, in which an endoscope is inserted for observation, usually takes 15 to 30 minutes. In addition, once polyps are discovered, the process from diagnosis to endoscopic surgery takes about 5 to 20 minutes.
However, the total time required from the time the patient arrives at the clinic to the time he or she returns home, including preparation before the examination (changing clothes, interview, etc.), recovery after the examination (a 30-minute to 1-hour break is required, especially if sedatives are used), and the physician's explanation of the results, should be estimated to be 2-3 hours in total.
These laxatives for colonoscopy are known as bowel-cleansing solution and are different from the laxatives usually prescribed for laxatives. Bowel-cleansing solution should be taken within an hour to flush out food in the gastrointestinal tract.
During this time, the patient has to go to the toilet 5-10 times, with little or no abdominal pain, although nausea and vomiting may occur, but this is also extremely rare.
We perform colonoscopy with a low-impact preparation of a plastic bottle (0.5 litter) of bowel cleansing solution and one litter of water.
We could perform painless colonoscopy without 2 litters of bowel-cleansing solution.
The clinic offers bowel cleansing solutions, three types.
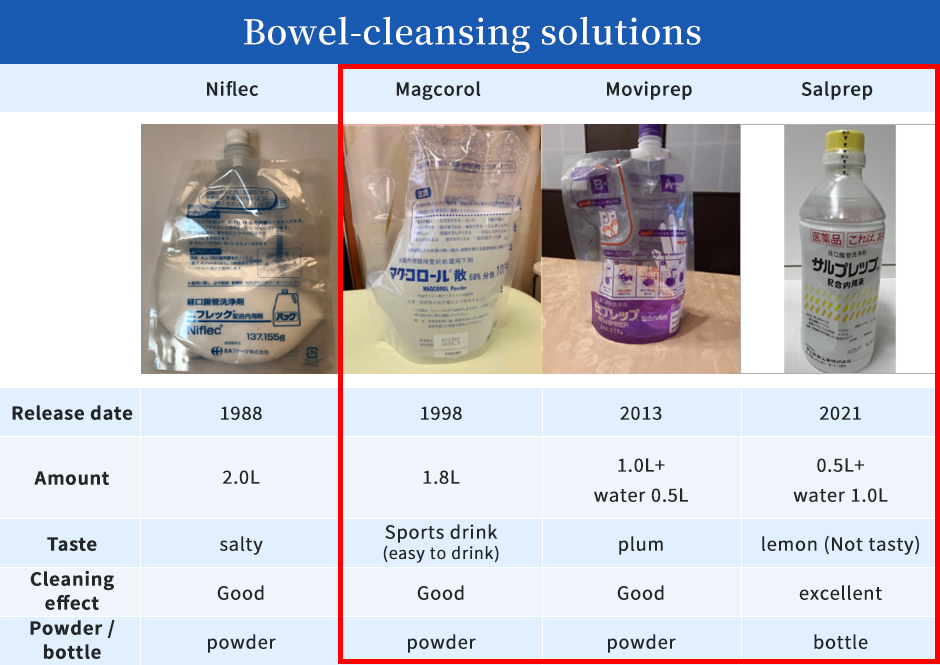
See table here (above).
Prior to the 1998s, bowel-cleansing solutions were 2.0 litters of laxatives in large quantities, and many people said they were difficult to drink.
The taste and quantity have improved over time.
Mobiprep and Sulprep require drinking 0.5 and 1.0 litters of water respectively within one hour, respectively, to prevent dehydration due to the high concentration of the bowel-cleansing solution. Sulprep is characterized by its excellent cleaning effect in small doses, but due to the high concentration of the solution, it has a rich taste and should be used with caution by people with kidney dysfunction. For those who do not like the rich taste, we recommend Magcoloric Acid, a sports drink-flavoured product that is relatively easy to drink. Mobiprep is used for people with renal dysfunction.
 The colonoscope is a long instrument measuring approximately 1 m 30 cm, and the scope is made of a soft tube to enter from the anus to the cecum. The colonoscope has a lens on the end of it, and the images captured by this lens are projected on a monitor for examination.
The colonoscope is a long instrument measuring approximately 1 m 30 cm, and the scope is made of a soft tube to enter from the anus to the cecum. The colonoscope has a lens on the end of it, and the images captured by this lens are projected on a monitor for examination.
The endoscope is approximately 11 mm thick, scope has a 3 mm tunnel for removing polyps and suctioning remaining stool in the intestinal tract, as well as a water supply port for letting air into the intestinal tract and for cleaning the lens, allowing polyps to be detected and even treated with a thin endoscope.

Colonoscopes vary in thickness, depending on their functional equipment.
The colonoscopic examination is mainly carried out using a 13.2 mm magnifying colonoscope at our clinic.
Magnifying colonoscope could observe magnification from normal to 100x. If a polyp is detected, the magnification can be immediately zoomed up to 100x for magnified observation to instantly diagnose whether the polyp is benign or malignant (cancerous) lesion. The light intensity is bright and the image quality is clear, enabling accurate diagnosis from lesion detection.
Generally, after a polyp is removed, patients spend nearly two weeks anxiously waiting for the pathology results, but the director, based on his experience studying pathology, is able to reassure them by giving them on the spot reliable results of benign or malignant conditions.
However, magnifying colonoscopes can be thick and rigid, and women with adhesions in the intestinal tract after gynecological surgery or a thin body may feel pain during colonoscope insertion.
If we start with an magnifying colonoscope but finds it difficult during insertion, the examination is possible immediately changed to another narrow colonoscope.
Painless colonoscopy is a prerequisite, and the colonoscope model is selected to suit the patient to ensure a painless and comfortable examination.
After cleaning the colon with bowel cleansing solution, the colonoscope is inserted through the anus and the endoscope is inserted into the cecum.
Once the cecum is reached, the colonoscope is slowly withdrawn and the inside of the colon is carefully observed.
If polyps or other lesions are detected, they can be magnified up to 100 times using a magnifying colonoscope for detailed observation.
Is it a benign polyp or early cancer that can be removed endoscopically? or an advanced malignancy (cancer) that requires surgery can be determined at that point.
This decision is very important.
The use of a magnifying colonoscope allows for accurate diagnosis.
This diagnosis could be performed with magnifying colonoscope and endoscopically resectable polyps are removed on the spot.
The treatment is carried out using newest equipment, so there are fewer post-treatment lifestyle restrictions than in the past.
Once you have had an colonoscopy, you would know when you need next examination.
In our clinic, diagnosis and treatment, i.e. endoscopic surgery, can be carried out in a single examination.
Colonoscopy is the most effective and reliable examination for the early detection of colorectal cancer.
In our clinic, colonoscopy polypectomies are performed as a day procedure and do not require hospitalization.
It requires a high degree of skill when inserted into the descending colon through the sigmoid colon, a tortuous intestinal tract.
If the sigmoid colon is folded accordion-style, the tortuous bowel is straightened and inserted into the descending colon, it is completely painless.
However, this maneuver requires a high degree of skill, and insertion techniques such as pushing the colonoscope through the sigmoid colon can make the examination torturous.
The colonoscopy can be performed as a completely painless examination if the intestinal tract is inserted in a straight line.
The clinic has received many positive reviews for its painless examinations, reliable diagnosis and appropriate treatment.
We are also confident that we can provide satisfactory colonoscopy.
Colorectal polyps are lesions that arise from the colonic mucosa, which has no sensory nerves.
Therefore, the excision is completely painless.
You can undergo endoscopic treatment without pain. Please be assured.
Previously, polyps were removed by applying an electric current, causing the excised wound to become a burn. Bleeding from damaged blood vessels could be seen in 0.5% of patients within 2-3 days after returning home, and life restrictions were required for 3-7 days after polypectomy.
Since April 2012, our clinic has been using a method of cold polypectomy for benign polyps of 10 mm or less, in which the polyps are removed without electricity. Therefore, there is little tissue damage after resection and little bleeding after returning home. The day after the resection, the patient is no longer restricted and can lead a normal life.
In lesions of suspected cancer less than 10 mm, depressed type tumors and polyps larger than 10 mm, electrosurgical excision (hot polypectomy) is indicated.
Life restrictions for hot polypectomy are 3 days to a week, depending on the size and shape of the polyps.
The following are lifestyle restrictions to prevent bleeding.
Avoid stimulant foods. Do not drink alcohol.
Avoid exercise (golf, jogging, etc.).
Baths should be showers for two to three days and avoid long baths after those three days.
The above must be observed for three days to a week.
Work can start the next day, but heavy lifting is discouraged for a week.
Ideally, it should be about a desk job.
The clinic uses sedatives and analgesics. No anesthetic is used.
Colonoscopy is performed in a state of low level of consciousness. Colonoscopy is completely painless if the colonoscopy is inserted using techniques that do not stretch the intestinal tract.
A high quality examination is only possible when the patient is conscious.
The colon has many flexures and it has been reported that cancer can be missed in these flexures.
It is important to change the patient's position to make it easier to see the flexure.
The change of position causes air movement, which inflates the flexure and makes it easier to observe.
This is necessary to ensure that cancer is not missed when performing the colonoscopy.
Furthermore, when a lesion is detected, a quiescent bowel is a good diagnostic and therapeutic aid for detailed observation of the polyp and endoscopic treatment.
To stop the bowel movement, we will ask to hold breath for a while.
At this time, the patient cannot cooperate if they are completely asleep.
For this reason, it is important to perform colonoscopy in a responsive and awake situation.
Our clinic do not use anesthetic agents.
Examination in a sleeping state using anesthetic medicine can be dangerous because the sensory nerves are also paralyzed and the patient is unconscious, so even if the intestinal tract is injured, the patient does not feel any pain.
In examinations when the patient is completely asleep, there is no cooperation from the patient, such as changing positions or holding the breath.
For a better and more accurate examination, a conscious state and moderate sedation will improve patient safety and quality of examination.
If a patient requests that the examination be carried out in a sleepy state, it is possible to carry out the examination in a relatively deep sleep, without anesthesia, but with sedatives suitable for the patient.
